Health
How Music Affects Your Baby’s Brain: A Mini Parenting Master Class

Discover how introducing music early can positively impact your child’s development. Music plays a significant role in a child’s growth, even before birth, and engaging with it early can support a healthy upbringing. We explored the effects of music on brain development and the origins of lullabies to understand how melodies shape a child’s cognitive and emotional growth.
The Impact of Music on Babies in the Womb
Research shows that music influences brain development even before birth. Listening to music during pregnancy not only soothes and uplifts expectant mothers but also positively affects the unborn child. By 16 to 18 weeks of pregnancy, a baby can hear its first sounds. By 24 weeks, rapid ear development allows the baby to respond to voices and noises. In the final months of pregnancy, babies can recognize their mother’s voice, native language, word patterns, and rhymes.
What Kind of Music Should Expectant Mothers Listen To?
In the third trimester, a baby can fully perceive external sounds, including music. Gentle, soothing melodies, such as classical music and lullabies, can have a calming effect. Music that evokes happiness can also contribute to a peaceful prenatal environment.
How Does Music Help Develop a Child’s Brain?
Music activates all areas of child development, particularly language acquisition and reading skills. Learning to play an instrument can enhance mathematical abilities and improve academic performance.
Using Music to Soothe a Baby to Sleep
Music elicits emotions and is often recommended as a tool to soothe babies. Incorporating calming music into a sleep routine can help babies settle peacefully. Slow, repetitive, and gentle tunes can slow the heartbeat and promote deeper, more relaxed breathing. A mother’s, father’s, or caregiver’s voice also holds unique power. Singing familiar tunes provides comfort, as a caregiver’s voice is soothing and reassuring to a baby.
The Origins of Lullabies
The word “lullaby” is believed to originate from the comforting “lala” or “lulu” sounds used to calm babies. The word “bye” may also be linked to its meaning, symbolizing a gentle goodnight. Lullabies, found in every culture and language, serve as soothing bedtime songs. Perhaps the most famous lullaby is Brahms’ Lullaby, recognized worldwide.
Best Musical Instruments for Toddlers
Creating music can be an enjoyable and accessible activity for children. The voice is the most natural instrument, but percussion sounds, such as clapping, snapping, and stomping, can also help introduce rhythm. Household items like wooden spoons and pots can be used to make music together. When choosing musical instruments for toddlers, options like toy drums, shakers, rattles, xylophones, and maracas are excellent choices for early musical engagement.
Can Music Help Your Child Socialize?
Listening to and playing music with others fosters a sense of connection and belonging. Music allows children to express emotions, communicate, and develop early social skills. Even infants respond to music by swaying, bouncing, and moving their hands rhythmically. Music also encourages language development as children mimic sounds, repeat words, and create their own songs. Studies suggest that music enhances empathy, trust, and cooperation by influencing brain circuits related to social bonding. This may explain why music has been a universal part of human culture.
Making Music a Part of Everyday Life
Music is woven into everyday experiences, from soothing a fussy baby to expressing joy and love. Parents instinctively use music to interact with their children, and by doing so, they support emotional and cognitive development. Introducing music to children from an early age nurtures their growth, enhances their social skills, and offers lifelong benefits. The sooner music becomes part of a child’s life, the greater its positive impact on their development.
Health
Uganda’s 2025 Ebola-Free Victory, Resilience and Global Prevention Lessons
Uganda was officially declared Ebola-free, marking the end of its sixth Ebola outbreak in just under three months.

Uganda was officially declared Ebola-free, marking the end of its sixth Ebola outbreak in just under three months. The outbreak, caused by the Sudan strain of the Ebola virus, began on January 29, 2025, in Kampala and affected five districts, resulting in 14 confirmed cases and four deaths. Uganda’s swift containment of this urban outbreak, despite challenges such as international aid cuts and the absence of approved vaccines, demonstrates a robust public health response and offers critical lessons for global Ebola prevention.
The outbreak was declared on January 29-30, 2025, after a 32-year-old male nurse died at Mulago National Referral Hospital in Kampala. The virus was confirmed as Sudan Ebola Virus Disease (SUDV) by three national laboratories and was genetically linked to a 2012 outbreak in Luwero, Uganda. Unlike the Zaire strain, which has an approved vaccine, the Sudan strain lacks licensed countermeasures, making containment reliant on public health measures and experimental trials. The outbreak spread to five districts being Kampala, Wakiso, Jinja, Mbale, and one other, posing a significant threat due to Kampala’s dense population of over 4 million. By February 7, 2025, new cases ceased, and the last patient was discharged on March 14, initiating a 42-day countdown. On April 26-28, 2025, Uganda’s Ministry of Health announced the end of the outbreak, a testament to the country’s experience with five prior Ebola outbreaks since 2000.
Uganda’s ability to contain the 2025 outbreak in under three months, its shortest Ebola response to date, was driven by a multi-faceted strategy:
Rapid Detection and Genomic Sequencing
Within 24 hours of the index case’s death, Uganda’s Central Public Health Laboratories confirmed the Sudan strain, and African scientists set a “world speed record” by sequencing the virus, tracing its origins back to the 2012 outbreak. This rapid diagnostic and genomic capability enabled an immediate outbreak declaration on January 30, 2025, activating emergency protocols.
Aggressive Contact Tracing and Quarantine
The Ministry of Health identified 265 contacts of the index case, placing them under strict 21-day quarantine in Kampala, Jinja, and Mbale. Mobile health teams and district task forces monitored contacts daily, preventing further spread. A surveillance gap, exposed when a four-year-old boy died undiagnosed on February 25, was swiftly addressed by intensifying tracing, adding two districts to the response. By February 27, most contacts had completed their quarantine.
Experimental Vaccine Trial
On February 3, 2025, Uganda launched a randomized clinical trial for a candidate SUDV vaccine at Mulago Hospital, using a ring vaccination approach to immunize contacts and contacts-of-contacts. Supported by the International AIDS Vaccine Initiative and WHO, the trial drew on lessons from the 2022 outbreak, demonstrating Uganda’s ability to integrate research into crisis response.
Isolation and Treatment
Confirmed cases were isolated at Mulago Hospital, with suspected cases triaged in temporary units. Supportive care, including rehydration and symptom management, was critical, as no approved SUDV treatments exist. Eight patients were discharged by February 19, and the last patient on March 14, with safe burial practices preventing transmission from the four deaths (two confirmed and two probable).
Public Health Measures
Uganda implemented point-of-entry and exit screenings at airports and borders, which were crucial given Kampala’s role as a transport hub. Community awareness campaigns via radio and local leaders educated the public on Ebola symptoms and prevention, countering misinformation. Healthcare workers used personal protective equipment (PPE), though supply shortages resulting from U.S. aid cuts were mitigated by WHO and local resources.
International and Local Collaboration
Local expertise was evident in Uganda’s laboratories and the Uganda Virus Research Institute, which supported diagnostics and trials. Internationally, the U.S. provided $8 million via the CDC and USAID, despite aid cuts that canceled four contracts, impacting screenings and PPE supplies. The WHO contributed $2 million and technical expertise, while the UN appealed for $11.2 million to support seven high-risk districts. Uganda shared genomic data regionally, aiding preparedness amid Marburg outbreaks in Tanzania and Rwanda.
Urban Setting: Kampala’s high population density risked rapid spread, but targeted interventions in five districts prevented a wider epidemic.
Aid Cuts: The Trump administration’s freeze on USAID funding strained surveillance and PPE supplies, but local and WHO support helped offset this shortfall.
Surveillance Gaps: The delayed diagnosis of a child emphasized the need for improved surveillance, which was quickly addressed through intensified efforts.
By overcoming these challenges, Uganda showcased resilience and innovation in its public health response, setting an example for global health efforts against Ebola and similar infectious diseases.
Features
Why Artists Turn to Drugs

The dream starts brightly: a song, a stage, a legacy. For countless artists, it’s a fire that burns hot until it doesn’t. Take Josh not his real name, but a true soul who’s been there. Fresh from university with a Bachelor’s degree in Industrial and Fine Art, he didn’t settle for a cubicle. “I wanted to create everything,” he says, his voice steady but heavy with memory. “The music, the videos, the designs, I’d be the whole machine.” As a songwriter and producer, he plunged into the industry, hunting for the hit that would make his name. But the climb was slow, and the years bled into each other as he sold beats for pennies and stacked unreleased songs that gathered dust.
By the age of 30, Josh had little to show but a few indie tracks and a growing ache from time lost. Then COVID hit, silencing the world and his hustle. Gigs vanished, pitched songs stayed shelved, and depression crept in like a shadow. “I was fighting wars that weren’t mine,” he says, “caught in industry politics, losing allies over things I couldn’t fix.” Drugs slipped in quietly not as inspiration, but as a way to mute the regrets piling up. “I should’ve taken that job after school,” he admits. “It would’ve kept me fed while I figured this out.”
Josh’s story isn’t unique, it’s a refrain echoed across the creative world, from bedroom studios to sold-out arenas. In Uganda, whispers circulate about Geosteady, the Afrobeat star behind “Owooma” and “Tokendeeza.” claiming he’s in rehab hint at a battle with addiction. It’s unconfirmed, just speculation, but it fits the pattern of an artist under pressure, teetering on the edge. Whether true or not, it raises a lingering question: Why do so many artists turn to drugs?
The answers aren’t simple, but they’re rooted in the crucible of the creative life. The pressure to produce is relentless, each track becomes a gamble on relevance, and every year without a win is a weight on the soul. For Josh, it was the grind of waiting for a break that never came. Research supports this; the Journal of Substance Abuse Treatment links high-stress creative fields to substance use as a coping tool. The National Institute on Drug Abuse adds that mental health struggles like the depression and anxiety Josh faced double the odds of reaching for a fix.
The culture plays a part as well. Music scenes can feel like a nonstop party, where drugs are as common as the beat drops. “It’s just there,” Josh says. “You don’t always choose it, it chooses you.” And then there’s the myth of the “tortured artist,” suffering for art’s sake. Society consumes this notion, think Hendrix, Winehouse turning pain into legend. But Josh shakes his head. “It’s not art, it’s survival. You’re not creating better; you’re just hurting less.”
For Josh, the spiral may have looked like depression feeding substance use, a diagnosis too common among artists. The instability of the gig economy, the emotional toll of rejection, and the quiet despair of “what if” nudged him toward escape. Alcohol could have been the start; harder substances, a deeper dive. Recovery meant stepping back. “I got a job and it was nothing fancy, just steady,” he says. “I wrote on my terms. Therapy helped when I could get it.” Not every artist has that lifeline; access to support varies, and in places like Uganda, resources can be scarce.
This story isn’t new, but it’s human. It’s Josh, staring down a decade of “what ifs.” It’s the whispered rumors of a star like Geosteady, whether true or not. It’s the push and pull of creation and collapse, played out in studios and souls worldwide. “I wish I’d known it didn’t have to be all or nothing,” Josh reflects, holding a quiet hope for those still in the fray. For every artist teetering on the edge, the prayer is that the music doesn’t fade to silence but rises again, stronger.
Blog
A Growing Ebola Threat in Uganda and How to Stay Safe
On January 29, 2025, Uganda’s Ministry of Health declared an outbreak of Sudan virus disease (SVD), a deadly strain of Ebola. This marked the country’s eighth encounter with this hemorrhagic fever since 2000.
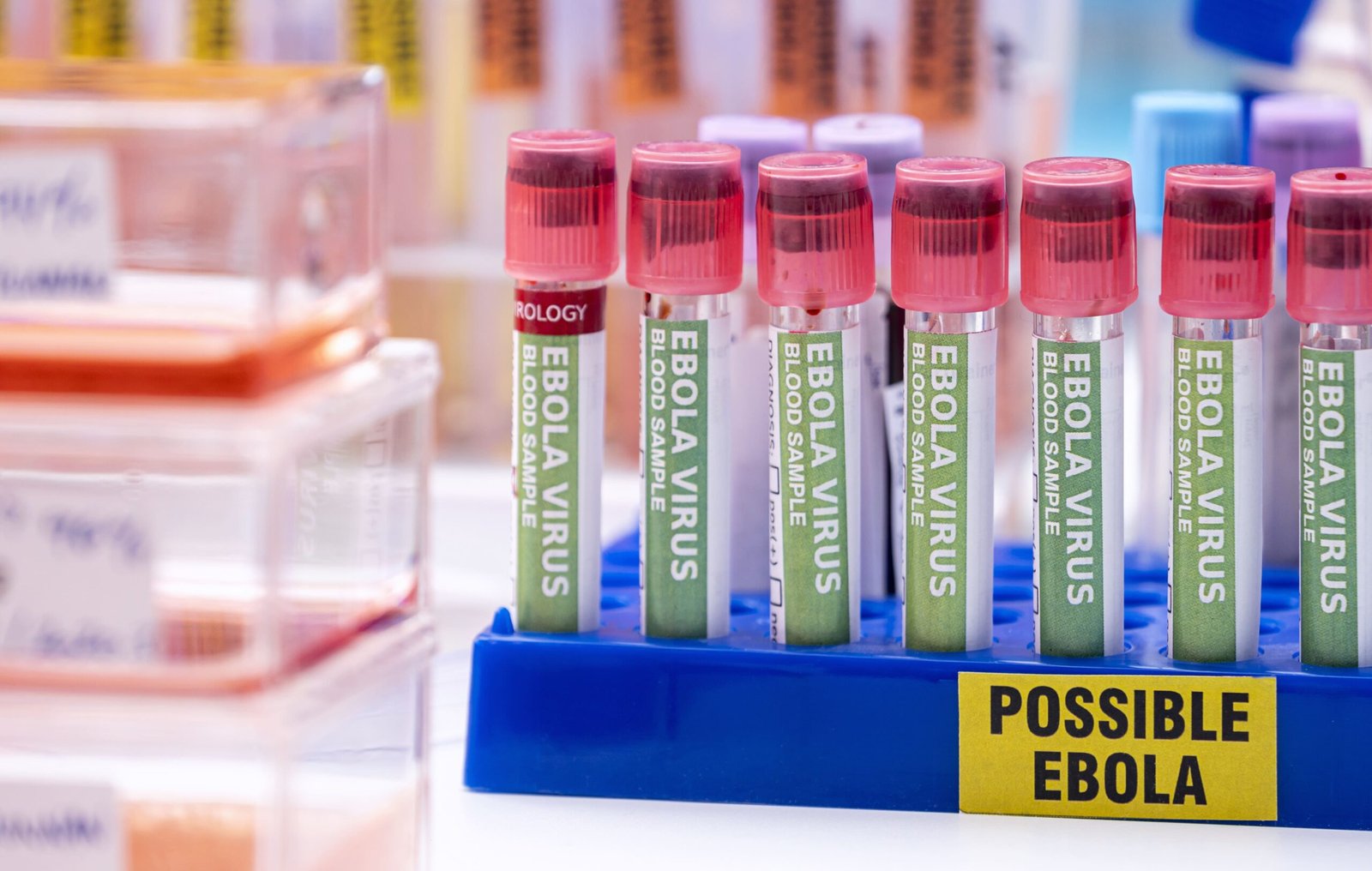
On January 29, 2025, Uganda’s Ministry of Health declared an outbreak of Sudan virus disease (SVD), a deadly strain of Ebola. This marked the country’s eighth encounter with this hemorrhagic fever since 2000. The outbreak began in Kampala, the bustling capital, when a 32-year-old male nurse died from the virus at Mulago National Referral Hospital. His death raised alarm bells because he sought treatment across multiple districts like Kampala, Wakiso, and Mbale. He even consulted a traditional healer, potentially spreading the virus before it was identified. As of March 18, 2025, the outbreak has caused multiple fatalities and tested Uganda’s resilience, but there are glimmers of hope amid the international response.
By March 5, 2025, the World Health Organization (WHO) reported 14 cases, 12 confirmed and 2 probable spanning six districts: Kampala, Jinja, Kyegegwa, Mbale, Ntoroko, and Wakiso. Four deaths have occurred, yielding a case fatality rate of 29%, which is lower than the historical average of 41% to 70% for the Sudan strain. The victims range from a 1.5-year-old child to a 55-year-old adult, with a mean age of 27 and a slight male majority (55%). A notable cluster of cases emerged in late February when a child under 5 died at Mulago Hospital, linking to additional infections.
The outbreak remains tied to a single transmission chain, with no spread beyond Uganda’s borders. As of March 17, there were no patients in care, and no new cases had been confirmed since March 2 raising cautious optimism that the worst may be over. If no further cases emerge, the outbreak could be declared over by mid-April, 42 days after the last exposure.
Uganda’s response has been prompt, utilizing experiences from its 2022 Ebola outbreak, which ended in January 2023 after 164 cases and 77 deaths. Within four days of the 2025 outbreak’s declaration, WHO and partners initiated a groundbreaking vaccine trial on February 3, utilizing a candidate from IAVI. This ring vaccination strategy targets high-risk contacts, marking a first in testing efficacy against Sudan virus disease during an outbreak. Experimental treatments, including a monoclonal antibody and remdesivir, are also undergoing clinical trials. By March 5, 192 new contacts were under surveillance, while 299 had completed a 21-day monitoring period.
International support has been critical. WHO allocated $3 million from its Contingency Fund for Emergencies, and Sweden contributed approximately $2 million (7.3–7.5 billion Ugandan shillings) to bolster Uganda’s efforts, likely aiding vaccine and containment initiatives. However, challenges persist. The absence of an approved vaccine or treatment for Sudan virus disease, combined with reported cuts in U.S. foreign aid under the Trump administration, has strained resources, according to U.S. officials on March 7.
Ebola spreads through direct contact with bodily fluids ie.blood, saliva, sweat, or vomit from an infected person or via contaminated surfaces. While Uganda’s outbreak is localized, understanding prevention is vital, especially in affected areas or for travelers. Here’s how to stay safe:
- Practice Good Hygiene: Wash hands frequently with soap and water or use an alcohol-based sanitizer. Avoid touching your face, especially your mouth, nose, and eyes.
- Avoid Contact with Sick Individuals: Stay away from anyone showing symptoms like fever, vomiting, diarrhea, or bleeding. Ebola is most contagious when symptoms are severe.
- Handle Animals with Care: Ebola can originate from wildlife such as bats or monkeys. Avoid handling bushmeat or wild animals, especially if they are sick or dead.
- Use Protective Gear: Healthcare workers and caregivers should wear gloves, masks, and gowns when near patients. Properly dispose of contaminated materials.
- Stay Informed: Follow updates from Uganda’s Ministry of Health or WHO. Avoid rumors and rely on verified sources.
- Seek Medical Help Early: If you experience fever, fatigue, muscle pain, or bleeding after potential exposure, isolate yourself and contact a health facility immediately.
Community education and contact tracing are crucial to Uganda’s strategy, emphasizing the importance of reporting symptoms and avoiding traditional practices like touching the deceased during burials, which have fueled past outbreaks.
The Ebola outbreak in Uganda in 2025 highlights both the danger of emerging diseases and the power of coordinated action. The vaccine trial offers hope for a future tool against Sudan virus disease, while Sweden’s aid and WHO’s leadership demonstrate global solidarity. For Ugandans in affected districts, vigilance remains essential. Washing hands, avoiding risks, and heeding health advisories could be the difference between containment and catastrophe. As the world watches, Uganda’s efforts may shape how we tackle Ebola for years to come.
-

 Entertainment5 months ago
Entertainment5 months agoMuseveni’s 2025 Copyright for Musicians breakdown
-

 Business5 months ago
Business5 months agoUganda’s Ministry of Finance projects significant growth opportunities in 2025
-
 Policies5 months ago
Policies5 months agoBreakdown of the Uganda Police Force Annual Crime Report 2024
-

 Health5 months ago
Health5 months agoBreaking down the Malaria Vaccine Rollout in Uganda
-

 Entertainment5 months ago
Entertainment5 months agoIsaiah Misanvu Teams Up with Nil Empire for a Soul-Stirring Anthem of Gratitude and Transformation “Far Away”
-

 Sports4 months ago
Sports4 months agoThe Transformative Impact of World Cup Qualification for Uganda
-

 Policies5 months ago
Policies5 months agoIs Uganda’s Shs10m Fine the WORST Thing for Cohabiting Couples?
-

 Business5 months ago
Business5 months agoUber and Lyft are finally available in all of New York State







